The Fall That Changed Everything: My Grandmother, Hidden Risk, and Why I Started Moviq Health
A Life Full of Strength and Independence
For most of her life, my grandmother kept excellent health. Her gait looked steady, her posture upright, her energy abundant.
When asked, she always said, “I’m doing well.”
She enjoyed visiting friends, cooking meals, laughing with family, and even taking occasional trips. She was only 78 years old.
Even as a physical therapist, when I observed her, I saw someone who looked remarkably good for her age. But appearance can be deceiving.
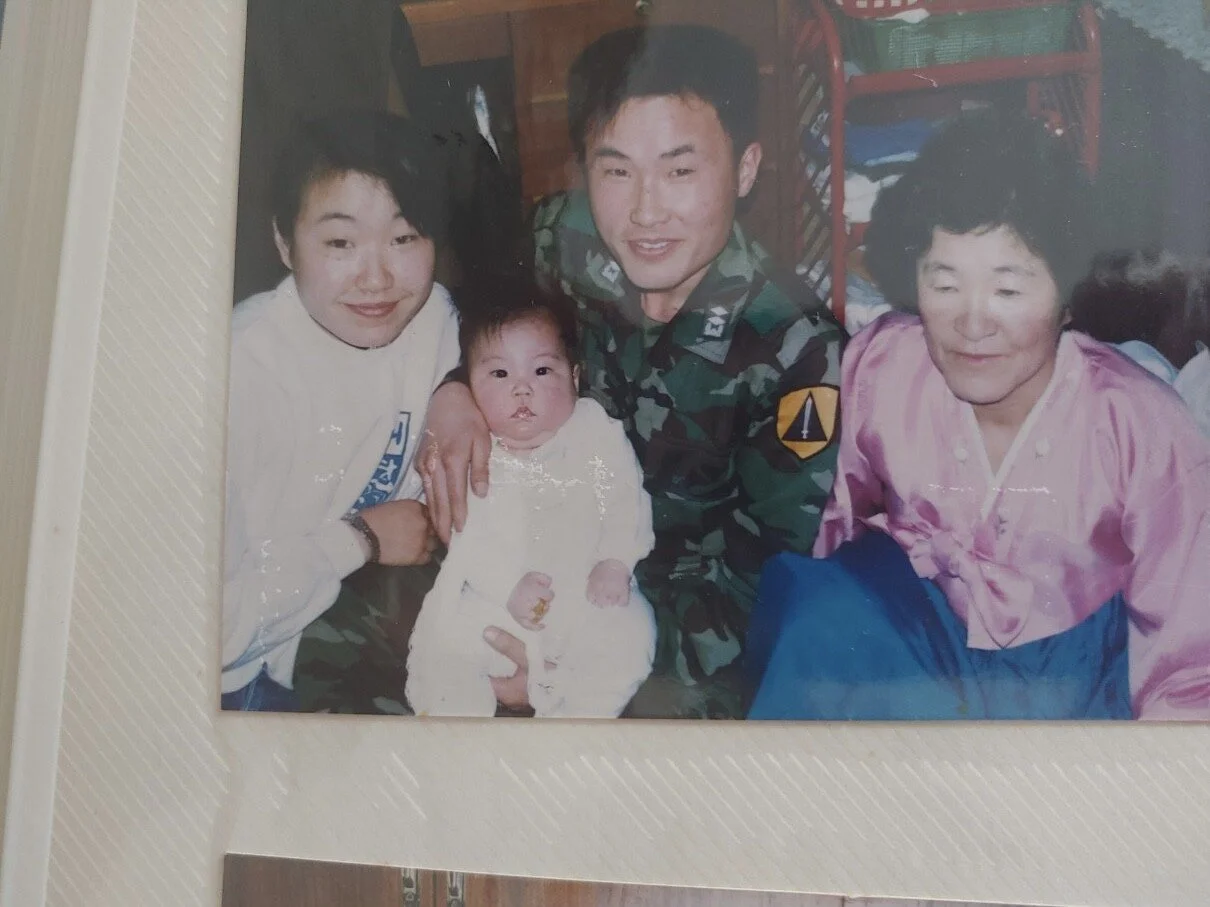
My grandmother in the middle before her fall in 2021
The Night Everything Changed
It was a normal afternoon in August 2023. She got up to use the bathroom. She missed a step, lost her balance, and fell.
She called my uncle immediately, who came to assist her. She was found on the living room floor, unable to move.
At the hospital, the X-rays confirmed a hairline fracture of her left hip.
For many older adults, a hip fracture is not just an injury. It’s an inflection point. Roughly 50% of older adults never regain their prior level of function after such an event. Many lose independence permanently.
For my grandmother, the decline was rapid. Surgery, hospitalization, rehab, and then bedbound living. The lifestyle she loved such as meeting her sisters, walking outside, traveling were suddenly impossible.
The Signs We Missed
Looking back now, the signs were there.
She needed more time walking the same distance.
She started using armrests to get out of a chair.
She occasionally used handrail to walk up and down the stairs.
Her confidence was not what it had been five years earlier.
These were not dramatic red flags. They were subtle changes, easy to dismiss, even for a trained physical therapist like me.
And here is the problem: our current healthcare system for classifying fall risk is fundamentally flawed.
The Systemic Failure
In healthcare, fall risk is typically identified through questionnaires and basic mobility screens such as asking a patient to walk down the hallway, standing on one leg, or verbally asking how their gait is.
By the time someone is classified as “moderate to high risk,” the opportunity for prevention and intervention are gone.
In essence, our healthcare system intervenes too late.
We fail to detect those subtle changes early, the ones that precede decline and falls. Subtle shifts in gait speed, stride length, double stance time, or force transfer during walking are often invisible to the naked eye, but they are measurable with the right technology.
My grandmother “looked fine.” She told everyone she was “doing well.” Even I, as her grandson and a licensed PT, missed the underlying decline.
Why Falls Are Not Just Accidents
Falls are not simply “accidents.” They are predictable, measurable, and preventable in many cases.
One in four adults over 65 falls every year.
Falls are the leading cause of injury-related deaths among older adults.
Hip fractures carry up to a 30% one-year mortality rate.
Yet, we treat falls as inevitable consequences of aging rather than signals of systemic failure.
Healthcare pours resources into treatment after the fall: surgeries, rehab, nursing care. But we invest far less in proactive detection and prevention.
The healthcare system is far more effective at preventing conditions like heart attacks and diabetes because it consistently monitors key indicators such as blood pressure, cholesterol, blood glucose, and HbA1c.
In contrast, mobility and functional abilities are often treated as an afterthought, rarely prioritized in the same proactive way by the healthcare system.
The Spark Behind Moviq Health
After my grandmother’s fall, I couldn’t shake one question:
What if we had known? What if the subtle changes had been detected earlier? What if intervention had happened six months before that night in August 2023?
That “what if” is why I created Moviq Health.
We are on a mission to build the first Movement Intelligence Platform that leverages clinical biomechanics to detect fall risk earlier than traditional screeners.
We focus on:
Objective data captured with high precision technology
Detect subtle changes in gait, strength, and balance that precede decline and falls
Risk classification: Moving beyond vague “low/moderate/high” categories toward dynamic, continuous scores to progress over time (scores ranging from "0 to 100")
Tests that are fully instrumented, standardized, & repeatable and not influenced by the provider's experience or skills.
Early intervention: Enabling clients and caregivers to act before decline becomes catastrophic.
Why Traditional Screenings Fail
Traditional fall risk assessments often rely on:
Visual Observation: Two providers may describe the same person’s gait differently
Stopwatch Tests: Only capture duration, not the quality of movement
Questionnaires: Depend on what patient's memory, perception, and their willingness to share
These methods of assessments unfortunately can produce a "passing" result even when underlying risk is present, which is exactly what happened with my grandmother.
The science of biomechanics provides a clear lens. Small increases in double stance time, reductions in ground reaction force, or irregularities in gait/cadence or postural sway reveal the story long before a fall occurs.
But until now, these insights stayed locked in research labs.
A Personal Reckoning
As a physical therapist, I’ve worked with countless patients after injuries and falls. I’ve seen the aftermath of falls, the struggle to regain independence, the frustration of families.
But it’s different when it happens in your own family.
The guilt is real. The thought that I “should have known.” The reality that even with my training, I couldn’t protect my grandmother.
That guilt is what I carry into Moviq Health, not as shame, but as motivation.
Because the system failed my grandmother, and it is failing millions of others.
My grandmother in 1991
From Pain to Purpose
The experience crystallized my conviction that we need to rewrite the rules of aging.
Independence should not end with a fall.
Families should not be blindsided by decline that “looked fine.”
Prevention should not be a luxury but the standard of care.
Moviq Health exists to give older adults a better future than my grandmother had.
We cannot change what happened to her. But we can change what happens for others.
Building a New Standard of Care
At Moviq Health, we envision a world where:
Every older adult gets objective, standardized, and repeatable fall risk assessments like the way they get their lab testing done.
Subtle decline is detected months or years earlier, giving time to intervene.
Data drives personalized exercise prescriptions to target specific preventative guidance.
Fall prevention is seen not as “optional wellness” but as core healthcare.
This is more than technology. It is a redefinition of what it means to age with dignity.
Why I’m Sharing This Now
I never intended to share my grandmother’s story publicly. It is painful, raw, and personal.
But I realize that hiding it does no justice to her or to the millions of families walking the same road.
Her fall changed everything for her. But it also changed everything for me.
It pushed me from observation into action. From frustration into innovation. From personal grief into collective purpose.
Her life before and after the fall is the reason Moviq Health exists.
If you are reading this as a clinician, caregiver, or policymaker, I ask you to join me in challenging the status quo. If you are reading as a family member of an older adult, I ask you to pay attention to the subtle changes.
Falls are not random accidents. They are preventable failures of our current system. And together, we can rewrite that story.