
The Science
High-resolution biomechanical data powering early detection and measurable outcomes in fall prevention.
The Problem
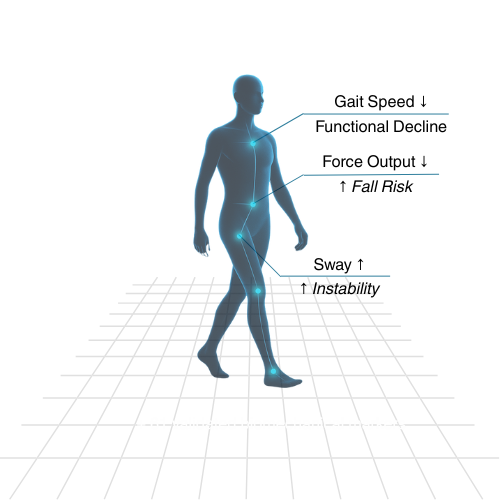
The Slow Decline behind Every Fall
Falls are the end result of a gradual loss of strength, balance, and coordination that builds quietly over time. The failure to measure movement precisely is what leads to the fall statistics we see today.
Adults 65+ fall each year,
affecting 14M Americans
Average hospital cost per fall-related inpatient visit
The leading cause of fatal &
non-fatal injuries among older adults
Scientific Foundation
Movement decline precedes falls, and science shows it.
Biomechanical Research
- ✔ Slower gait speed is linked with higher risk of disability, hospitalization, and mortality in older adults.Studenski S. JAMA (2011)
- ✔ Decline in power and force precede falls by years, making them ideal early signals.Trombetti A. Osteoporos Int (2016)
- ✔ Objective sway and limits-of-stability testing expose risks not visible in questionnaires.Quijoux F. Physiol Rep (2021)
- ✔ Slower gait, shorter stride length, and longer double support distinguish fallers from non-fallers.Silva J. Biomechanics (2024)
- ✔ Lower-limb power tests outperform simple stopwatch tests in predicting injurious or recurrent falls.Zhu Z. BMC Geriatrics (2025)
Detecting movement decline is the foundation of fall prevention.
Scientific Continuum
From Sports Science to Everyday Care
The same technology once reserved for athletes is now transforming how we prevent falls. By applying sports science to everyday care, we can detect small, measurable decline in force, balance, and coordination that precede falls.
Sports Science
- ✔ Optimize technique, speed, and power
- ✔ Reduce injury risk and time-loss
- ✔ Tools: motion capture, force plates, wearables
- ✔ Metrics: gait, force output, stability
- ✔ Outcome: improve performance & extend career longevity
Moviq Health
- ✔ Optimize strength, balance, and coordination
- ✔ Reduce fall risk and hospitalization
- ✔ Tools: gait capture, force plates, balance plates
- ✔ Metrics: gait, force output, balance
- ✔ Outcome: improve mobility & extend independence

Our Scientific Approach
Your movement is as unique as your fingerprint, and we measure your movement with precision.

Like a fingerprint, gait may look similar from a distance, but detailed biomechanical analysis reveals patterns unique to every individual.
That’s why measuring your movement with precision is so important for preventing falls. Because subtle deviations from your movement pattern can signal early decline long before a fall happens.
Quantifying Movement
Moviq Health captures your movement with millisecond-level and single-degree precision, converting detailed data into a personalized fall risk profile.
Predictive Intelligence
Our predictive modeling transforms your biomechanical datasets into foresight, enabling early intervention before falls.
Clinical Precision
With a 2.7% test–retest variance, it means your biomechanical data can be trusted to reflect true changes in your movement, not random noise or measurement error.
Internal Validation
The Foundation of Predictive Modeling
Cohort
- 84 adults ambulating without assistive devices
- Ages 50+
- Community-dwelling, able to consent, no acute musculoskeletal injuries
Protocol
- 64 biomechanical markers captured across gait, force, and balance
- 3D gait capture, force plate, and balance plate
Follow-up and Outcome
- Single follow-up at 12 months via SMS or email
- Outcome measured as number of falls in the past 12 months
- Only falls that resulted in the person making contact with the floor were counted.
Preliminary Findings
- Expected falls of the cohort = 9.64
- Actual number of falls of the cohort = 11
- Test–retest variance = 2.7%
Clinical Impact
Data-Driven Fall Prevention
✔ Validated Predictive Accuracy: Our predictive model can forecast fall incidence over 12 months, demonstrating strong agreement between predicted and observed outcomes.
✔ Precision-based Prevention: Enables detection and intervention of early losses in strength, balance, and coordination before a fall occurs.
✔ Early Awareness: Moviq Health identifies the smallest changes in your movement to reveal the earliest signs of decline. You will see exactly how your strength, balance, and gait are trending, allowing you to act early.
Future Plans
Expanding the Science of Fall Prevention
Predictive Model Expansion
We plan to develop an AI/ML model that forecasts the number of falls a person may experience within twelve months. The model draws on biomechanical patterns across gait, balance, and strength to refine prediction accuracy.
Peer-Reviewed Publication
We plan to publish a peer-reviewed research paper that demonstrates Moviq Health’s clinical validity in a larger-scale study. The findings will establish objective biomechanics as a powerful tool for early detection of mobility decline and fall prevention.
Clinical Partnerships
Moviq Health is forming collaborations with hospitals, rehabilitation networks, and research institutions to bring objective biomechanics into preventive care. These partnerships will help make clinical biomechanics testing part of everyday health.
Continuous Innovation
Future developments will enhance our testing systems and create real-time feedback analytics. These advancements will make fall prevention continuous, connected, and personal.
References
- National Council on Aging. Falls Prevention. Published 2025. Accessed October 15, 2025. Available at: https://www.ncoa.org/older-adults/health/prevention/falls-prevention/
- Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi:10.1001/jama.2010.1923. Available at: https://jamanetwork.com/journals/jama/fullarticle/644554
- Trombetti A, Reid KF, Hars M, et al. Age-associated declines in muscle mass, strength, power, and physical performance: impact on fear of falling and quality of life. Osteoporos Int. 2016;27(2):463–471. doi:10.1007/s00198-015-3236-5. Available at: https://pubmed.ncbi.nlm.nih.gov/26194491/
- Quijoux F, Nicolaï A, Chairi I. A review of center of pressure (COP) variables to quantify standing balance in elderly people: algorithms and open-access code. Physiol Rep. 2021;9(24):e15158. doi:10.14814/phy2.15158. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC8623280/
- Silva J, Atalaia T, Abrantes J, Aleixo P. Gait biomechanical parameters related to falls in the elderly: a systematic review. Biomechanics. 2024;4:165–218. doi:10.3390/biomechanics4010011. Available at: https://www.researchgate.net/publication/378763364_Gait_Biomechanical_Parameters_Related_to_Falls_in_the_Elderly_A_Systematic_Review
- Zhu Z, Zuo JJ, Li K, et al. Association of lower-limb strength with different fall histories or prospective falls in community-dwelling older people: a systematic review and meta-analysis. BMC Geriatr. 2025;25:685. doi:10.1186/s12877-025-05685-3. Available at: https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-025-05685-3
